Moreover, that’s just the start. There are a lot of hard numbers reflecting a real need for added support in medical imaging. And as the figures below show, that represents an opportunity for the global medical community to lean further into radiologist-led, AI- and ML-backed solutions that enhance decision-making.
1. The shortage is global, and disparities are broad.
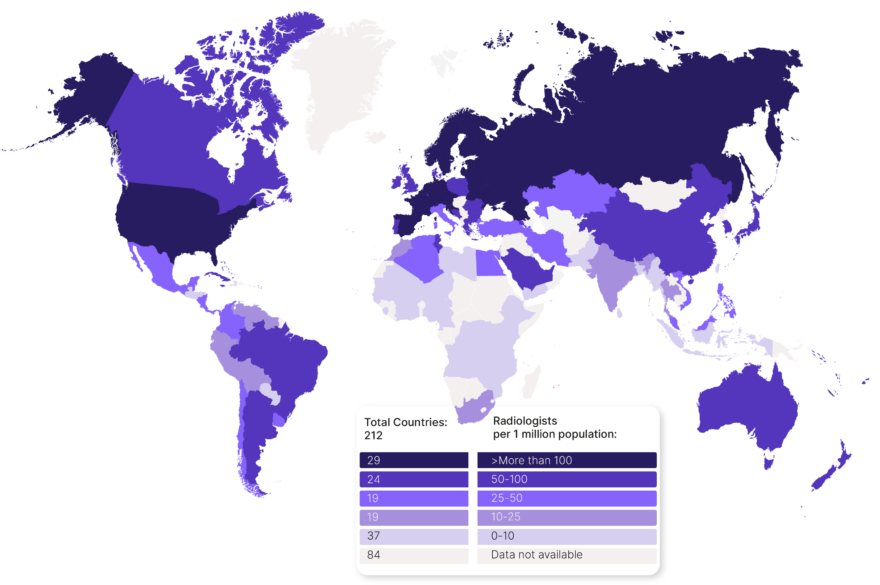
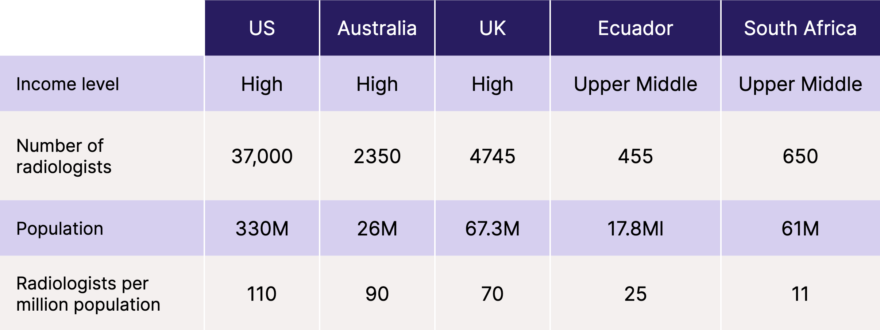
Simply put, one’s country of residence can have a significant impact on their access to medical imaging. Information shared by the International Atomic Energy Agency (IAEA) breaks the disparity down by the country’s income level, with analysis indicating:
- In the US and across most of Europe, people have access to 100+ radiologists per one million residents.
- Contrast this with countries such as Indonesia, Sri Lanka, Paraguay & Pakistan where it is reported there are less than ten radiologists per million inhabitants.
Such low numbers per million essentially means large swaths of patients are locked away from the radiological care they need. And looking deeper even IAEA’s high income countries continue to talk about the shortage in such blunt terms where seemingly “high” numbers of radiologists per million might not be enough.
2. An ageing population will need more radiology services.
In Australia, persons over 65 were “the largest users of diagnostic imaging, representing 38.5% of all examinations” in 2021 per data National Institute of Health (NIH) website. Likewise, cohorts are thought to spend increasing amounts on radiology services with age until they reach the 80-85 age range.

Combined with WHO projections that the number of people over 60 worldwide will double by 2050, it’s easy to see the trend at play. Already the largest user of radiology services and growing exponentially in size, an ageing population will undoubtedly require more radiology services than the medical training system can currently output.
3. Not enough trainees and lengthy training times.
It takes approximately 11-13 years or longer to fully train a radiologist in many medical systems worldwide, including the US, Australia, and the UK. And these figures from the Radiological Society of North America (RSNA) illustrate the supply and demand disparities between trainees entering the field & requirement of services:
…] from 2010 to 2020, the number of diagnostic radiology (DR) trainees entering the workforce increased just 2.5% compared to a 34% increase in the number of adults over 65.
There are no shortcuts when producing trained medical professionals. Instead the need falls to tools that can redefine the end-to-end radiology workflow.

4. Vacancy rates are increasing & we have an ageing talent pool.
Gaps in the workforce are continuing to grow to worrying depths in the UK, a workforce shortage of 29% in 2022 is projected to grow to 40% by 2027 according to the 2022 RCR census report, and current training supply will not meet demand. By 2027, an additional 3,365 clinical radiologists will be needed to keep up with service need – a 70% increase on the current workforce. The report also expresses concerns with the number of specialists leaving the field:
While the number of consultants joining the workforce has remained in line with the five-year average, the number of consultants leaving is considerably higher. Concerningly, 76% of consultants (whole time equivalent) who left the workforce in 2022 were under the age of 60.
The UK’s approximate projected increase in vacancy rate between 2022-2027 isn’t the only one of note. In the US, per this ACR bulletin, of the 20,970 radiologists engaged in active patient care, over 80% of radiologists are 45 and up; and 53% are age 55 and over. As they point out, “The current radiologist population is skewed toward seasoned professionals who may be looking at retirement.”

Although the challenges facing each nation may differ in nature, the outcome remains the same – workforce growth is not keeping pace with demand, with worrisome potential outcomes in medical imaging.
5. Outsourcing is a substantial (but necessary) drain on resources.
The UK spent some £178m (approx. US$230m, AUD$339m) on “insourcing, outsourcing, and ad-hoc locums in the UK during 2020-2021” details the 2021 RCR census report. This is equivalent in cost to some 1,876 full-time salaries – half the crown’s available workforce. This figure soared to £223m (an increase of 25%) in it’s latest census report from 2022.
Direct outsourcing figures for other countries are harder to source, but supporting data and publications suggest similar issues abound. In the US, for instance, the medical imaging outsourcing industry as a whole is expected to grow to a US$10.6 billion industry, up from US$7.25b in 2019.
While the UK’s outsourcing moves and costs have arguably grabbed the most headlines, the larger story looks like a global industry doing what it can to shift dwindling resources from one spot to another. While outsourcing will always be a part of the healthcare world, imaging needs comprehensive decision-support help to shore the gap.

6. Around half of radiologists report burnout.
Burnout creates staff shortages, and radiologists in the US—per research sourced in RadioGraphics—report it at a high rate: 49%, with other resources reporting it at an even higher global rate of 54%. Numbers coming from other countries tell much the same story; for example, in Australia and New Zealand radiologists reported burnout rates as high as 49% all the way back in 2010.
In the UK, 100% of clinical directors are concerned about morale, stress and burnout among their workforce according to the 2022 RCR Census. RCR also conducted a survey among its members to assess their wellbeing and levels of burnout. The findings made for interesting reading with many considering reducing their working hours, some having already done so. Approximately half of those surveyed reported being burnt out, and a further 33% said they were slightly burnt out.
In the face of these alarming burnout statistics among radiologists, the integration of AI technologies offers a promising solution to alleviate this pervasive issue. AI-driven tools have the potential to significantly enhance the efficiency and accuracy of radiological tasks, allowing radiologists to focus their expertise on complex cases and critical decision-making. By automating routine tasks such as image analysis and initial anomaly detection, AI can free up valuable time and mental energy for radiologists, reducing their workload and mitigating burnout risks.

Shaping the future of healthcare through cutting-edge tools
Medical imaging doesn’t need more of the same outlook in a changing healthcare world – current radiologists need support, just as their graduating colleagues will as they matriculate into the workforce.
The tools we’re building at Annalise.ai show a viable, smart, and emerging way around the shortfalls. The accelerated growth in medical imaging has raised expectations on radiologists and healthcare providers, to diagnose patients accurately and at speed. To relieve this pressure while creating meaningful change takes a pioneering blend of clinician-led thinking and technological capabilities.
As the healthcare industry continues to embrace AI innovations, there is a compelling opportunity to reshape the landscape of radiology, fostering improved well-being for radiologists while ensuring optimal patient outcomes.
We’d love to show you more about this growing industry and its ability to help bridge the ever-increasing gaps in radiology, subscribe below to keep up to date with developments in AI and healthcare. Or head to Annalise.ai to find out more about our multi award-winning decision-support AI tools for chest X-ray and head CT.